Brushing and flossing every day will help keep your teeth and gums healthy.
Having clean teeth also makes you look and feel better. Your breath is fresher, brighter,
and your teeth feel smooth.
How to brush

- Brush after meals, using a soft toothbrush and a fluoride toothpaste. Start in one
place and work all the way around your mouth. Brush the front, back, and top of each tooth as explained below.
- Hold the brush at a 45 angle and gently brush the outer surfaces, circular and/or back and forth motion.
- Brush the inner surfaces of the back teeth using the same circular back and forth motion.
- Turn the brush and use the tip to clean the inner surfaces of the upper and lower front teeth.
- Clean the chewing surfaces using a scrubbing motion. Brush then rinse well.
How to floss
- Floss at least twice a day to remove plaque between the teeth and below gums.
Start at one place and work all the way around your mouth. Floss between each
tooth as explained below.
- Wrap 18 inches of floss around your middle fingers. Secure it with fingers
and thumbs.
- Ease the floss between your teeth. Press it against one side, then wrap to
form a C shape.
- Work the floss back and forth, and up and down, going below the gums where
plaque collects.
Note:
- If you have a bridge or wear braces, use a floss threader to get the floss under the
bridge or the wires.
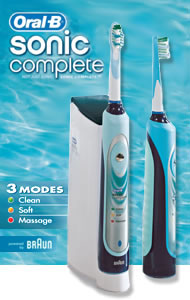
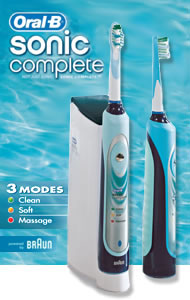
The electric toothbrush has been marketed since the 50's, designed for everyone.
It works well for patients with special problems, like excessive bleeding, periodontal
disease, or poor manual dexterity.
What are the advantages of an electric toothbrush?
- Remove plaque bacteria, twice as much as the manual toothbrush.
- Ability to clean in hard to reach places like between teeth and far back teeth.
- Reverse the effect of gingivitis, such as bleeding gums.
- Remove light stains, such as coffee and tobacco.
- Especially maintains good oral hygiene.

What is gum disease?
- Gum disease is an inflammatory disease that attacks the gums, bone and other
supporting structures causing loss of teeth. Gum disease is caused by plaque,
a sticky colorless film of bacteria that continuously forming on the teeth.
Plaque contains potentially harmful bacteria. Plaque irritates the gums,
causing them to become red, tender and swollen. It causes the gums to
bleed easily, a condition called gingivitis. Also, your body defends
itself against bacteria by producing increased level of enzymes which begin
to break down tooth and gum tissue. Eventually, the tissue that attaches
the gums to the teeth is destroyed by the irritants in plaque. The gums
pull away from the teeth and small pockets form between the teeth and
gums. These pockets become filled with more plaque. Eventually, the jawbone
supporting the teeth is destroyed, a condition called periodontitis.
- Periodontal disease is usually a slow, painless, and progressive disease.
Most adults with gum disease are unaware that they have it. If diagnosed
early the teeth can be saved.
Contributing factors:
In addition to plaque, a number of factors cause gum disease including:
Physical and chemical irritants
Impacted food, smoking, chewing tobacco, excessive
alcohol consumption, improper use of dental floss and toothpicks.Oral conditions that cause abnormal stress on mouth tissues
Badly aligned teeth, poor fitting bridges or partial dentures and defective
fillings; also habits such as grinding, clenching the teeth and chewing ice.Unbalanced diet
Evidence shows a link between nutritional deficiency and the body's
ability to fight off infection. Vitamin C deficiency has been linked to gum disease.Pregnancy
Increased hormone levels may aggravate a condition commonly referred to as
pregnancy gingivitis.Diseases
Diabetes, uremia, liver cirrhosis, anemia and leukemia may affect the health
of your gums.Certain medications
Oral contraceptives, antiepilepsy drugs, steroids and cancer
therapy drugs may also affect the gums.
What are the signs?
- Gums that bleed during brushing and flossing.
- Red, puffy and tender gums.
- Gums that have receded or separated from the teeth.
- Pain when chewing.
- Calculus or tartar build up.
- Teeth that seem loose or that change position.
- Changes in your bite.
- Changes in the way your partial dentures fit.
- Persistent bad breath or a bad taste in your mouth.
- Teeth that are overly sensitive to hot and cold.
Treatment:
- Scaling and root planing removes the tartar and the soft tissue lining the
periodontal pocket. This helps eliminate the inflammation and reduce the pockets and restore gingival health.
Gingivectomy is the surgical removal of the soft tissue wall of a pocket to eliminate the depth of the pocket.
Flap surgery allows access to the root of the tooth for removal of calculus, plaque
and diseased tissue. The gum is then sutured back into place.
Helpful Tips:
- Practice appropriate home care such as brushing and flossing at least twice a day.
Eat a well-balanced diet.
- Examine your mouth routinely for any early signs of gum disease or other oral changes.
Visit your dentist at least twice a year for a thorough cleaning and oral examination.
Incidence and survival:
- Oral cancer will be diagnosed in an estimated 30,000 Americans every year, and will
cause approximately 8,000 deaths. On average, only half of those with the disease will
survive more than five years.
What is the importance of early detection?
- With early detection and timely treatment, death from oral cancer could be
dramatically reduced.
- Early detection of oral cancer is often possible; tissue changes in the mouth that might
signal the beginning of cancer can often be seen and felt easily.
What could be the warning signs?
Possible signs and symptoms of oral cancer that might be noticed are:
- Leukoplakia (white lesions).
- Erythroplakia (red lesions).
- Lump or thickening in the oral soft tissues.
- Difficulty chewing or swallowing.
- Difficulty moving the jaw or the tongue.
- Numbness of the tongue or other areas in the mouth.
If the above problems persist for more than two weeks, a clinical and laboratory test
is necessary for a definitive diagnosis.
What are the risk factors?
- Tobacco, especially chewing tobacco, and excessive alcohol use increases the risk of oral cancer.
- Exposure to the sunlight is a risk factor to the lips.
- Oral cancer is typically a disease of older people.
- Oral cancer strikes men twice as much as it does women.
Treatment:
- Surgery to remove the cancer in the mouth.
- Radiation therapy, which is a high-energy ray, is used to kill cancer cells.
- Chemotherapy, which is the use of drugs to kill cancer cells.
Oral piercing is a growing trend, which include piercing the lip, tongue, and other oral tissue in the mouth.
What are the risk factors associated with oral piercing?
- Airway obstruction from swallowing the jewelry.
- Chipped teeth.
- Speech impediment.
- Swelling and bleeding.
- Blood poisoning.
- Nerve damage.
- Keloid scaring.
- Promote the spread of Hepatitis B, C, Aids, and STDs.
What are the measures that you should take before oral piercing?
- Have the piercing done by a professional.
- Make sure the instruments used are sterilized.
- Choose the right design, size, and material of jewelry.
- Practice good oral hygiene around the pierced area.
- Ear piercing guns are never appropriate for oral piercing.
Root canal is the treatment of the diseased nerve (also called the pulp) of the tooth.
A root canal treatment enables you to save and keep your original damaged tooth.
What makes a root canal necessary?
- Physical irritation caused by deep decay or a very large filling
- Severe gum disease
- Crack in the tooth.
- Trauma, such as physical blow to a tooth or a constant striking of a tooth in the opposite jaw that traumatizes the tooth
Regardless of the initial cause, the tooth pulp becomes stressed and infected.
Bacteria grows within the tooth pulp, causing pressure and pain, sometimes accompanied
by swelling of the area. Sometimes the deterioration of the pulp happens so gradually
that little pain is felt. Either way, eventually the infection can destroy the pulp
and spreads to the bone and surrounding tissues causing abcess at the root tips.
What are the steps of the procedure?
- Once it has been determined (with X-rays and clinical examination)
that the root canal treatment is necessary, you will be scheduled for
one or more appointments. It's important that you keep these
appointments, in order to prevent delays in treatment and healing.
- The tooth may be isolated with a piece of rubber dam. This
confines the treatment area and protects the mouth from bacteria
and chemical agents that will be used to clean the root canal.
- After isolating the tooth, the, canals will be cleaned, enlarged
and shaped using hand files, or rotary instruments.
- The canals will be washed and cleaned using different chemical agents.
- One or few x-rays might be taken to ensure all the measurements
and that the walls inside the canal are smooth.
- Then, the root canal will be permanently filled using root canal
sealant. or in some cases, a temporary medication will be placed
inside the tooth to control bacterial growth and reduce infection,
and the root canal will be filled in your next appointment.
- A temporary filling is placed in the opening of the tooth
until next visit.
- Finally, in your next visit a post will placed inside the canal
to strengthen it and the tooth will be crowned (capped) and fully restored
to chewing function.
What care follows the treatment?
Brittleness
A non vital tooth is more brittle than a vital one and
is more susceptible to fracture. Therefore, in most cases,
it is recommend that your root canal tooth be crowned
(capped) following treatment.Discoloration
You may notice that your treated tooth (especially a
front tooth) might change color. Be sure to ask your
dentist about tooth whitening if the tooth is
not restored with a crown.
Helpful Tips:
- Don't chew on the treated tooth for 48 hours.
- Take the medication prescribed by your doctor.
Snoring is a common problem that people might not be aware of. It can be defined as a
loud breathing sound during sleep that is caused by the vibration of the soft palate
(the soft part of the roof of the mouth). Snoring is normal, but in rare cases can be
a sign of a serious medical problem like sleep apnea.
What are the main causes of snoring?
- Not known cause.
- Chronic nasal congestion.
- Too much alcohol or sedation.
- Obesity.
- Enlarged adenoids and tonsils.
- Sleep apnea (episodes of no breathing).
What can I do to reduce snoring?
- Avoid sleeping on the back.
- Weight loss can reduce snoring.
- Avoid drinking alcohol before bedtime.
- Using an appliance can help, like snore guard.
- Always check with your health provider.
People often grind their teeth in their sleep. You may not even know you're doing it.
The causes are not clear. Stress is one possible cause, but often the reason for the
habit is not known.
Symptoms of grinding:
Your dentist may ask whether you have certain symptoms such as:
- A sore, tired jaw
- Dull headaches
- Earaches
- Sensitive teeth
Symptoms like these may be a signal that you grind your teeth.
Treatment:
Mouth guards:
A mouth guard is a plastic device that fits over your
teeth. It protects them from grinding damage. A mouth guard
is worn at the times when you're most likely to grind
you teeth.Stress Reduction:
Stress is suspected in many cases of bruxism. Reducing
stress may help relax your jaw muscles and make
grinding less likely. Your dentist may suggest regular
exercise or other ways to reduce stress.Medication:
In some cases medication may be given. It may help relieve
sore muscles or reduce stress.Fixing damaged teeth:
Your dentist can discuss ways to fix teeth damaged by
bruxism. Crowns and onlays are two ways to fix
damaged teeth.
Teeth sensitivity is a common problem that faces many people every day. Because of
the discomfort involved, especially in brushing, some people tend to avoid the sensitive
areas. This may result in complicating the problem.
What causes teeth sensitivity?
- Root sensitivity (exposed root surface) usually occurs after gum recession or gum treatment.
- Tooth abrasion (loss of tooth enamel at the gum line).
- Tartar control toothpaste will sometimes cause teeth to be sensitive.
- Old and poor fitting fillings.
- Cavities.
- Occlusal trauma.
What can be done to reduce teeth sensitivity?
- Check with your dentist to find the cause and get the proper treatment.
- Fluoride treatment.
- Proper brushing techniques using soft toothbrush.
- Use desensitizing toothpaste.
- Decrease the intake of acid-containing food and liquids.
What is teeth whitening?
- Whitening (bleaching) is a simple procedure that can be done at the dentist office
or at home. During the procedure a solution of hydrogen peroxide is applied to lighten
the discolored and darkened teeth.
What causes teeth discoloration?
- Tetracycline (antibiotic) staining
- Excessive fluoride
- Trauma (injury) to the teeth
- Pulp (nerve) degeneration
- Restorations (silver, gold)
- Genetic and acquired illnesses
- Aging
- Food, drinks (such as coffee and tea), and tobacco.
Another consideration in determining whether tooth whitening
is for you is the condition of your teeth. Careful clinical
examinations and x-rays will help determine whether you
are a candidate for this procedure.
Does whitening (bleaching) damage the teeth?
- No. When the active whitening agent comes in contact with water, hydrogen peroxide is
released, which whitens the teeth. Bleaching does not weaken or soften the teeth.
Can I bleach my teeth during pregnancy or while nursing?
- It is always recommended as a precaution measure to not use bleaching products during
pregnancy or while nursing.
What happens during at-home tooth whitening?
Your teeth are examined:
Before you begin at-home bleaching, your teeth must be
clean. Any gum problems need to be treated. Any cavities
must be filled, and old fillings may need to be replaced.Your molds are made:
Models of the teeth will be made.You receive your trays and gel:
You will be shown how and when to use the trays and bleaching
gel, how many days you will need to use the bleaching
gel depends on how badly discolored the teeth are.
What happens during in-office tooth whitening?
Your teeth are examined:
Before you begin in-office bleaching, your teeth must be clean.
Any gum problems need to be treated. Any cavities must be filled, and old fillings may
need to be replaced.Your teeth are bleached:
A piece of rubber dam might be used to isolate the teeth,
a whitening gel will be applied to the teeth, and an ultraviolet light will be used
to accelerate the whitening process, that will take about ten minutes, the teeth after
that will be washed an cleaned, the procedure will be repeated 6-8 times till the
desired shade is reached.
What are the advantages of in-office tooth whitening?
- Safe and simple procedure.
- Fast and can be done in one hour.
- Limited sensitivity.
Are over the counter whitening products safe?
- Many of these products are too abrasive, and can damage the teeth with extended use.
Supervision by your dentist is the safest way to whiten your teeth.
Helpful tips:
For best results, follow these tips:
- Brush and floss your teeth before placing in the bleaching trays.
- Follow your dentist's directions exactly, and use only the materials your dentist gives you.
- Spit out any excess saliva. The bleach won't harm you if swallowed, but it can irritate your throat.
- Don't eat or drink while you have the trays in your mouth.
- Rinse your mouth out well after bleaching.
- Avoid citrus fruits and other acidic foods, they can make your teeth more sensitive.
- Call your dentist if your throat, teeth, or gums feel irritated.
What is TMJ?
- The temporomandibular joint (TMJ) is a joint that connects the jaw bone to the skull
and is located just in front the each ear. It is a sliding ball and socket, it is one
of the most complex joints in the body.
What are the signs of TMJ disorder?
- Noises associated with the movement of the jaw (clicking, popping, or crunching).
- Pain when the jaw is opened wide.
- Ear pain not related to ear infection or ear ringing.
- Clenching or grinding teeth.
- Limited mouth opening.
- Frequent headaches.
What causes TMJ disorders?
TMJ disorder may develop for any number of reasons:
- Lost or crooked teeth.
- Overbite.
- Malocclusion (teeth that fit together poorly).
- Head and neck injuries.
- Clenching or grinding teeth.
- Degenerative arthritis.
Treatment:
- If malocclusion is diagnosed, teeth may require restoration, crowns, or orthodontic treatment to correct and improve the bite.
- If grinding or clinching teeth diagnosed a splint may fabricated to fit the teeth and separate the upper and the lower teeth slightly, patient may be instructed to wear the splint at day time or only when sleeping.
- Relaxation and psychological consulting are important to relieve the stress and anxiety; physical therapy can help to exercise the jaw and relief any tension in the muscles, medication and ultrasound therapy can provide significant relief of symptoms for many patients.
- When arthritis is present, various procedures are performed to repair or replaced severe or perforated discs and smooth the bone surfaces.
- Only in small cases surgery is required to correct TMJ disorders.